The Invisible Ingredient
How the West Outsourced Its Medicine Cabinet — and Why Getting It Back Will Be Slower and Costlier Than Anyone Admits
You likely have a bottle of pain relievers or antibiotics in your bathroom cabinet.
It sits there, mundane and unassuming, next to the toothpaste and the extra razor blades.
You trust that if you or your child gets sick, those pills will be there.
You trust that if you drive to the pharmacy with a prescription in your hand, the pharmacist will hand you a white paper bag with the medicine that makes the pain stop.
But take a closer look at that white tablet.
The label on the bottle might say it was “Manufactured in New Jersey” or “Packaged in Ohio.”
It might even have a comforting, familiar brand name that you have known since childhood.
But that label is only telling you a partial truth and it is the less important half of the story.
The actual engine of that pill—the chemical powder that makes it work—almost certainly traveled thousands of miles to get to you.
It likely began its life in a massive industrial park in China.
It traveled on a container ship across the Pacific, sat in a customs warehouse, was trucked to a processing facility, and finally pressed into the shape you recognize.
We have built our modern health system on a supply chain we cannot see.
Do not control
And barely understand.
For thirty years, this invisible system worked perfectly.
It was a marvel of globalization, delivering life-saving medicine to the world at prices so low they were almost negligible.
A course of antibiotics cost less than a sandwich.
A generic blood pressure pill cost pennies.
We assumed this was the natural order of things.
But as 2025 draws to a close, that illusion is starting to break down.
The trade wars, the shipping blockades, and the silent diplomatic standoffs of the last twelve months have revealed a terrifying reality: the West may own the patents and the brand names, but they rely heavily on China for the ingredients or APIs/KSMs.
To understand how we lost control of our own medicine cabinet, you have to look past the finished pill and understand the “baking” process of chemistry.
Think of it like baking a cake.
To make a cake, you need flour, sugar, and eggs.
If you have the best oven in the world—the most expensive, high-tech, stainless-steel convection oven—but you have no flour, you have no cake.
You just have a hot metal box.
In the pharmaceutical industry, the United States and Europe have the best ovens.
We have the high-tech factories that take powders, mix them with binders and coatings, and press them into tablets. We have the FDA inspectors who ensure the factories are clean.
We have the logistics networks that truck the bottles to CVS and Walgreens.
But China owns the flour.
In the industry, this “flour” is known as the Key Starting Material (KSM). These are the raw chemical building blocks that are reacted together to create the Active Pharmaceutical Ingredient (API).
The API is the drug itself.
It is the molecule that kills the bacteria or lowers your cholesterol.
Everything else in the pill is just packaging.
While Western companies were busy marketing the finished “cakes” and fighting over patent rights for the next billion-dollar blockbuster drug, China quietly spent thirty years cornering the market on the flour.
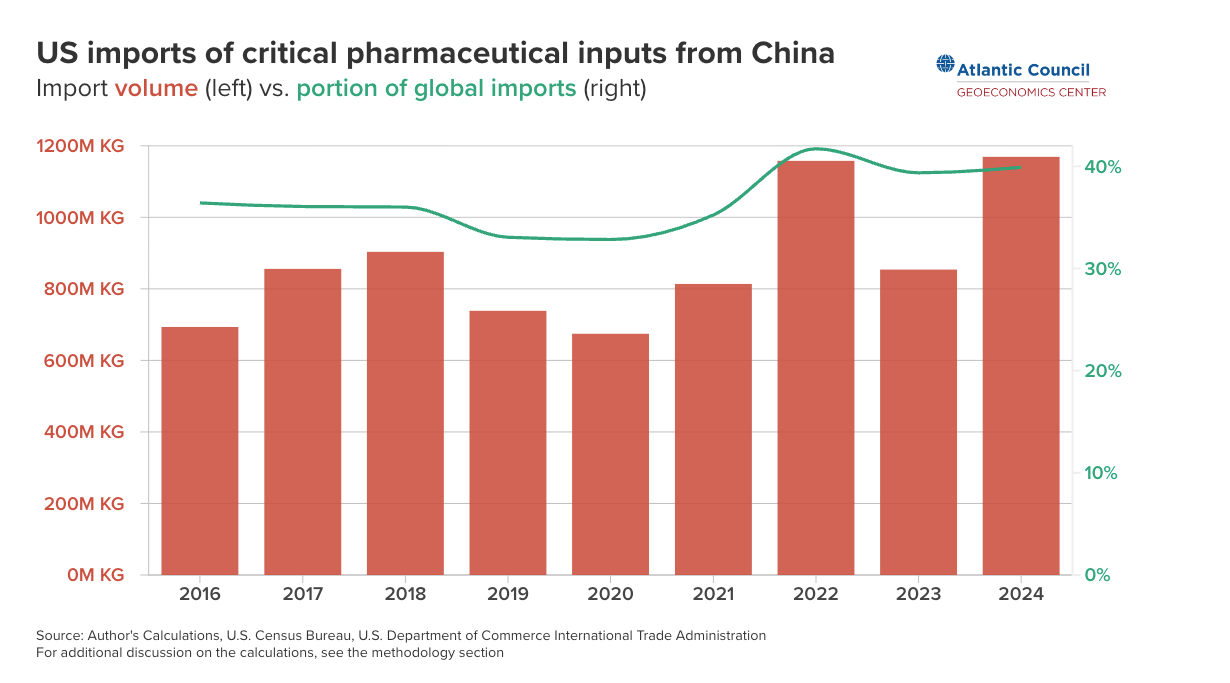
Today, a majority of the chemicals used to make generic drugs worldwide come from China.
That’s fine when countries get along, but it breaks down when geopolitical rivals try to squeeze out advantages from one another.
The Great Outsourcing
How did we get here?
How did the United States, the country that invented mass production and won World War II with its industrial might, lose the ability to make basic medicine?
It wasn’t a conspiracy.
It wasn’t a secret theft in the night.
It was a choice.
Specifically, it was a choice made by Western accountants and environmentalists in the 1990s and 2000s.
In the late 20th century, the United States and Europe maintained substantial capacity to produce essential medicines end-to-end.
Facilities handled fermentation, chemical synthesis, formulation, and packaging within relatively compact supply chains.
A key part of this ecosystem in the U.S. was Puerto Rico, which became a pharmaceutical manufacturing hub under Section 936 of the U.S. tax code.
What Was Section 936?
Enacted in 1976, Section 936 allowed U.S. corporations to operate manufacturing facilities in U.S. territories while paying little or no federal corporate tax on income earned there. The policy was designed to encourage economic development in places like Puerto Rico.
For pharmaceutical companies, Section 936 functioned as an industrial anchor.
It made it economically viable to locate high-value manufacturing — including fermentation and chemical synthesis — on U.S. soil, under U.S. regulatory oversight, while remaining competitive with overseas producers.
Puerto Rico became home to a dense cluster of pharmaceutical operations. These were not just packaging plants. They included upstream production, skilled technical workforces, and decades of accumulated institutional knowledge.
Critics argued that Section 936 amounted to corporate welfare. In the 1990s, amid budget pressures and a political environment hostile to tax incentives, Congress voted to phase it out beginning in 1996, with full expiration by 2006.
The decision was framed as fiscal reform, but its industrial consequences received far less attention.
As the tax advantage disappeared, so did the economic rationale for maintaining expensive, heavily regulated manufacturing in U.S. territories.
Medicine is Messy
As the US government was working to “reduce corporate greed” it was also beginning to recognize the importance of having a clean environment.
Making antibiotics is not like making an iPhone.
It is not a clean, dry assembly of parts.
It is closer to brewing beer or refining oil.
To make Penicillin or Amoxicillin, you have to ferment massive vats of broth filled with mold and bacteria.
It is a biological process.
It is messy.
It creates tons of waste that have to be treated and disposed of safely.
In the 1990s, the West began to tighten its environmental belts.
We wanted cleaner rivers and fresher air.
We passed strict regulations on chemical waste.
At the same time, the pressure to lower healthcare costs was mounting. Insurance companies and governments wanted cheaper drugs.
Then, China made the West an offer it couldn’t refuse: Let us do the dirty work.
Beginning in the late 90s, Beijing identified pharmaceuticals as a “strategic pillar” industry.
They didn’t care about the brand-name drugs that cost a billion dollars to invent. They cared about the volume.
They wanted to make the chemicals that everyone needs every day.
The Chinese government offered massive subsidies to build chemical parks.
They offered tax holidays.
And they looked the other way on pollution.
If a factory in China dumped chemical runoff into the local river, nobody came to shut them down.
This gave Chinese manufacturers a massive cost advantage.
They could produce the raw powder for Amoxicillin at a fraction of the cost of a factory in Tennessee.
Western pharmaceutical executives looked at the spreadsheets. The math was undeniable. If they shut down their expensive, regulated factory in the US and bought the powder from China, they could save millions of dollars a year.
They could boost their stock price.
They could deliver cheaper drugs to consumers.
It felt like a win-win.
The West got cheap medicine and cleaner environments; China got the jobs and the cash.
One by one, the Western factories closed.
The fermentation vats were dismantled and sold for scrap.
The skilled chemists who knew how to run them retired or moved on to other industries.
We saved pennies on every pill. But we lost something that doesn’t show up on a quarterly earnings report: Capacity.
We assumed that the world would always be friendly.
We assumed that global trade would always be free and open.
We assumed that we could always buy the flour, as long as we had the money.
We forgot the oldest rule of strategy: You cannot fight a war, or fight a disease, with inventory you don’t have.
The Trap Snaps Shut
Fast forward to 2025.
The friendly world of the 1990s is gone.
We are in a new era of Great Power Competition, and medicine has become a weapon.
The trade war that has dominated the headlines this year didn’t start with medicine. It started with electric vehicles, semiconductors, and tariffs.
But as tensions rose, the “weaponization” of supply chains moved from theory to reality.
Military strategists often talk about ammunition. They track how many missiles and bullets they have in reserve.
For the pharma industry they tracked their finished drug stockpiles, but they have made a critical mistake.
They tracked the bullets but ignored the gunpowder.
In the world of medicine, the United States makes the finished drugs, but China controls the “gunpowder”, the KSMs.
In late 2025, we saw what happens when the gunpowder runs low.
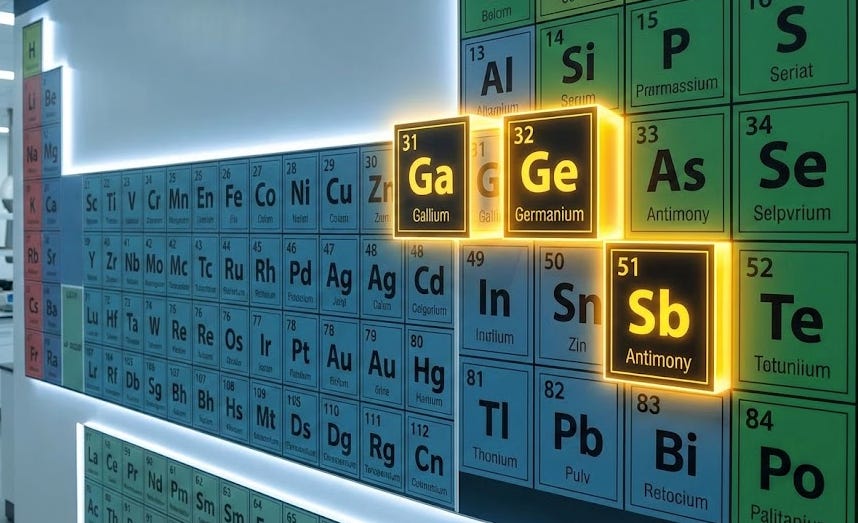
It started with Antimony.
You have probably never heard of antimony.
It is a silvery-white metalloid, element 51 on the periodic table.
It is used in fire retardants and lead-acid batteries.
But it has another critical use: it is a “fining agent” used to make high-quality, clear glass.
Specifically, the type of glass used for pharmaceutical vials, the little bottles that hold vaccines and injectable drugs.
China produces the majority of the world’s antimony.
When the trade war heated up this year, Beijing placed export restrictions on it.
It wasn’t a total ban, just a “licensing requirement.” But the effect was immediate.
The price of antimony in Europe and the US surged and glass manufacturers began to panic.
Then came the Gallium and Germanium restrictions, minerals used in semiconductors and advanced medical imaging machines.
Now we are starting to see antibiotic shortages.
In hospitals across the country right now, doctors are facing a scenario that feels like it belongs in the 19th century, not the 21st.
The pediatric wards are seeing a surge in winter respiratory infections. Strep throat, ear infections, pneumonia—standard, treatable illnesses.
For fifty years, the answer has been simple: Amoxicillin. It is cheap, safe, and effective.
But this winter, Amoxicillin is in short supply.
This isn’t because we forgot how make it.
It’s because the supply of the raw Amoxicillin powder has choked.
A combination of stricter environmental enforcement in China and the new export licensing rules has slowed the flow of the KSMs needed to make the drug.
This is the “Trap.”
We are so dependent on this single source that even a minor disruption causes a crisis.
And if things were to get worse, with a true “kinetic” conflict over Taiwan or the South China Sea, the flow would stop completely.
Experts testifying to Congress have warned that U.S. buffer stocks for some critical medicines can be measured in months leaving little margin when supply chains break
We would be a superpower with aircraft carriers and stealth bombers, but we would be unable to treat a simple infected wound.
The Clinical Reality
This problem is not confined to antibiotics that treat routine infections, nor is it confined solely to China.
Cisplatin is a platinum-based chemotherapy agent.
It is not new; it was approved in 1978.
It is generic and costs about $15 a vial.
Much of Cisplatin was produced in India specifically with a manufacturer called Intas.
Intas operated on the margins sourcing materials from China and then trying to operate on the razor thin margins that exist in the generic market.
A routine FDA inspection proved they were playing a little too lose with the rules and the FDA shut them down leading to a shortage of Cisplatin.
We are having to ration life-saving care in the wealthiest nation on Earth, not because the science doesn’t exist, but because we cannot buy a $15 generic chemical.
This happened in 2023, it happened in 2024, and it is happening again in 2025 with even greater intensity.
The “Just-in-Time” efficiency of the global supply chain has become a “Just-too-Late” reality for patients.
The fragility extends beyond cancer. It affects the most basic surgeries.
Anesthetics, muscle relaxants, saline solution—all of these rely on supply chains that are dangerously concentrated. A surgeon cannot operate without these basics.
If the supply of propofol (an anesthetic) is cut, the operating rooms go dark. The heart transplants, the hip replacements, and the emergency C-sections all stop.
The India Delusion
Whenever this topic is debated in Washington or London, someone inevitably raises a hand and says: “Why don’t we just buy from India? Isn’t India the ‘Pharmacy of the World’?”
It is true that India is a pharmaceutical giant.
By volume, India supplies about 40% of the generic drugs used in the United States. Walk into a CVS, and many of the bottles will say “Made in India.”
This gives policymakers a false sense of security.
They think, “Great, we have a backup. We aren’t dependent on China; we are diversified.”
This is a dangerous delusion.
India is the world’s pharmacy, but China is the world’s chemical plant. The Indian pharmaceutical industry is built on a foundation of Chinese inputs.
India imports the majority of its Key Starting Materials and APIs from China.
Indian manufacturers are painfully aware of this. They call it a “strategic chokehold.” During the border skirmishes between China and India in 2020, Chinese shipments of KSMs slowed down.
Indian drug manufacturers panicked and prices for raw materials skyrocketed overnight.
The Indian government is trying to fix this.
They have launched a massive “Production Linked Incentive” (PLI) scheme, pouring billions of dollars into subsidies to restart domestic production of things like Penicillin.
They are having some success.
In 2024, India restarted penicillin production for the first time in decades.
But the scale of the problem is immense.
China’s chemical industrial parks are cities unto themselves.
They have integrated power plants, waste treatment facilities, and state-subsidized raw materials.
They operate at a scale that is hard to comprehend.
For India to replicate that infrastructure will take a decade, not a year.
For the immediate future the “India Option” is not a true alternative.
If China turns off the tap, the Indian pharmacy goes dry just as fast as the American one.
The Long Road Home
So, what do we do?
The year 2025 has seen the first real, legislative attempts to fight back.
In the United States, the BIOSECURE Act has been the headline news.
This law is effectively a “divorce decree” for the biotech sector.
It prohibits the US government—and by extension, any hospital that takes Medicare or Medicaid—from contracting with “biotechnology companies of concern” linked to foreign adversaries.
The goal is to scrub the supply chain.
It forces US pharma companies to look at their suppliers and elimate any companies tied to the Chinese military or government.
Europe is following suit with its Critical Medicines Act, which aims to coordinate stockpiling and encourage local production.
These are the right moves. They are necessary moves. But they are also incredibly painful.
The problem is that you cannot rebuild an industrial base overnight.
You cannot simply flip a switch and bring the factories back.
First, there is the Time factor.
Building a pharmaceutical plant is not like opening a coffee shop.
It takes three to five years to design, build, and validate a facility.
The FDA has to inspect it.
The processes have to be tested for stability.
If we decide today to build a penicillin plant in North Carolina, the first usable pill won’t roll off the line until 2029 or 2030.
Second, there is the Cost factor.
This is the uncomfortable truth that nobody likes to talk about.
We outsourced these jobs because it was cheaper.
Bringing them back will be expensive.
Western labor is more expensive than Chinese labor.
Western environmental regulations are stricter.
Western energy costs are higher.
If we make Ibuprofen in the USA, it will not cost pennies per bottle.
It might cost dollars.
Are we willing to pay that?
For thirty years, we have trained consumers and healthcare systems to expect rock-bottom prices.
We have awarded contracts to the lowest bidder.
We have squeezed every ounce of profit out of the generic drug market.
To fix this, we have to change the economic model.
We have to be willing to pay a “security premium.”
We have to accept that a bottle of antibiotics costs $20 instead of $5, because that extra $15 is paying for a factory that follows environmental laws and is located in a friendly country.
It is paying for the assurance that the medicine will actually be there when we need it.
This is the great Medical conflict of the next decade.
It is a battle between Efficiency and Resilience.
Efficiency is cheap, fast, and brittle.
Resilience is expensive, redundant, and sturdy.
We spent thirty years worshipping at the altar of Efficiency.
Now, faced with empty shelves and geopolitical threats, we are rediscovering the value of Resilience.
The New Kitchen
The era of cheap, invisible medicine is over.
The “End of History”, that brief, optimistic period where we thought free trade would solve all conflicts, has ended.
We are back in history now, and history is messy.
The shortages of 2025 are a warning shot.
They are a mild taste of what a full decoupling would look like.
We have a choice to make.
We can try to patch the holes, sign temporary truces, and hope that the geopolitical storm blows over. We can keep buying the flour from our rival and hope they keep selling it to us.
Or, we can do the hard work.
We can rebuild the “kitchen.”
It will require a level of industrial policy we haven’t seen since the Cold War.
It will require the US, Europe, Japan, and India to work together, not as competitors, but as allies building a redundant network.
It will cost money.
It will raise the price of healthcare.
It will take a decade of effort.
But consider the alternative.
When the next pandemic hits, or a war breaks out, do we want to be left left holding the best ovens in the world, staring at empty cupboards?
You cannot bake a cake with promises.
You need ingredients.
For too long, we pretended that having the recipe was enough.
It isn’t.
We can not rely on hope that in the future, China will willing export the ingredients we need to make critical medicine.
We have to rediscover the ability to create the ingredients ourselves.
It is the only way to make sure the medicine we need, is there when we need it.